Quick Facts
Someone in the world is newly infected with tuberculosis every second.Target Markets
Our drug candidates have broad market potential with applications in Tuberculosis, Peptic Ulcer Disease and Gastric Cancer, Crohn’s Disease, Bacterial Pneumonia, and a number of other infectious diseases.
Tuberculosis
A highly contagious infectious disease, TB is caused by the bacterium Mycobacterium tuberculosis. TB is a global health problem with a large market potential in the established market economies (EME), where there are developed health payer systems that support the financial burden of treatment, as well as in 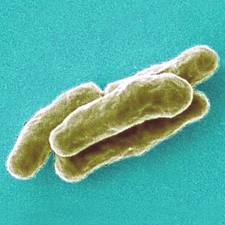 developing countries with growing market economies. According to the 13th annual TB report of the World Health Organization (WHO), there were an estimated 2 billion people infected with TB and 9.27 million new cases of active TB disease worldwide in 2007. Annually, approximately 1.6 million non-HIV infected people die of this disease and an additional 0.5 million HIV infected people also die of TB. The WHO projects that a staggering 70 million people worldwide will die of TB over the next three decades.
developing countries with growing market economies. According to the 13th annual TB report of the World Health Organization (WHO), there were an estimated 2 billion people infected with TB and 9.27 million new cases of active TB disease worldwide in 2007. Annually, approximately 1.6 million non-HIV infected people die of this disease and an additional 0.5 million HIV infected people also die of TB. The WHO projects that a staggering 70 million people worldwide will die of TB over the next three decades.
Specifically for our products, the current U.S. addressable TB-infected population for new TB drugs numbers roughly 365,000 potentially infected people (approximately 15,000 physician-reported active TB cases, 350,000 pediatric, latent and putative TB cases) treated in the private sector. In the EU and Japan, there are approximately 93,000 active TB cases (125,000 in the EU and 45,000 in Japan) that would benefit from improved TB therapeutic products. With these target populations and the current antiquated drug treatment regimens, there is a substantial commercial market for improved TB products in the EME. The current cost of treating an individual with drug-susceptible TB is approximately $25,000. This figure escalates to approximately $250,000 to treat MDR TB. According to the GATB, the current antitubercular drug market is estimated at $410-$470 million annually and will grow to well over $600 million by 2010, with a potential market for a new anti-TB drug that is approximately $316-$432 million.
Treatment
Sequella research and development efforts have generated the largest pipeline of new TB drugs in development.
The current recommended TB treatment regimen requires administration of four first-line TB drugs (Isoniazid, Rifampin, Pyrazinamide, and Ethambutol or  Streptomycin) for a minimum of 6 to 9 months. These TB drugs were developed between 1944 and 1970. According to the Journal of the American Medical Association (JAMA): “New drugs are needed to treat TB because the current drug combination has significant disadvantages.” (JAMA 2005; 293: p.2705) There is a need for TB drugs that require shorter treatment duration; work effectively against strains of drug-resistant TB bacilli; deliver an improved side effects profile; and help address medication compliance issues.
Streptomycin) for a minimum of 6 to 9 months. These TB drugs were developed between 1944 and 1970. According to the Journal of the American Medical Association (JAMA): “New drugs are needed to treat TB because the current drug combination has significant disadvantages.” (JAMA 2005; 293: p.2705) There is a need for TB drugs that require shorter treatment duration; work effectively against strains of drug-resistant TB bacilli; deliver an improved side effects profile; and help address medication compliance issues.
H. pylori Infection, Peptic Ulcer Disease and Gastric Cancer
Helicobacter pylori infection of the gastric epithelium is the most common bacterial infection worldwide. Its global prevalence is estimated at 50%, though the burden falls disproportionately on the developing world, where the prevalence in some areas is 80%. H. pylori infection is generally acquired during childhood, and without specific  antibiotic treatment can persist for life. The infection is generally clinically asymptomatic during childhood, and even in adulthood 80-90% of infected individuals will remain asymptomatic (although they may transmit the bacteria).
antibiotic treatment can persist for life. The infection is generally clinically asymptomatic during childhood, and even in adulthood 80-90% of infected individuals will remain asymptomatic (although they may transmit the bacteria).
Approximately 10%-20% of infected individuals eventually develop peptic ulcer disease. Both gastric and duodenal ulcer disease are strongly correlated to H. pylori infection: approximately 95% of duodenal ulcers and 85% of gastric ulcers occur in the presence of H. pylori infection, and the lifetime risk for developing ulcers is 3-10-fold greater in those infected with H. pylori. Eradication of H. pylori with antibiotic therapy nearly completely prevents ulcer recurrence.
H. pylori is the only bacterium causally linked to the development of cancer. Several studies have demonstrated that H. pylori seropositivity is associated with a 2.1 to 16.7-fold increased risk of gastric cancer. Of those infected with H. pylori, 1-2% will develop distal gastric adenocarcinoma, the second leading worldwide cause of cancer related-death. A total of 700,000 people die of this cancer each year, and the 5-year survival rate in the U.S is <15%. Eradication of H. pylori in infected individuals who do not yet have pre-malignant lesions has been shown to significantly decrease the risk of developing cancer.
Treatment
H. pylori infection is recalcitrant to therapy with a single antibiotic. Thus, the standard guideline for the treatment of this infection consists of at least seven days of triple-therapy (clarithromycin and either amoxicillin or metronidazole, and a proton pump inhibitor, PPI).
Early studies attributed an efficacy with this regimen of slightly less than 90% to 95%, depending on the study. However, more recently, success rates have decreased to 75% to 80% in some areas of the world.
Whether due to antibiotic resistance or one of several other mechanisms, clinicians are left with relatively few, less than adequate choices to treat H. pylori infections, including H. pylori-associated duodenal ulcer disease, and gastric cancer.
SQ109 is a new, small molecule antibiotic with characteristics that make it particularly attractive to evaluate against H. pylori as it orally bioavailable, acid-stable, has in vitro activity against H. pylori, and achieves high intracellular concentration (which may be important to effect bacterial eradication).
Crohn’s Disease
Crohn’s Disease (CD) is a chronic and painful recurrent inflammatory disorder of the intestines that is accompanied by unpredictable bouts of diarrhea, bowel adhesion and obstruction. Long considered an autoimmune inflammatory disorder, current CD therapies (steroids and anti-inflammatory biologics) treat symptoms of overactive inflammation in the gut.
Like many chronic diseases today, evidence is mounting that CD has a currently unrecognized infectious origin. A major suspect for etiologic agent is the NTM M. avium paratuberculosis (MAP). People with CD have 7:1 odds of having a documented presence of MAP in blood or gut tissues than those without CD. MAP also causes Johne’s disease of cattle and ruminants, a disease with similar symptoms as CD.
Treatment
SQ641 is the lead drug candidate from a 7000-compound library of semi-synthetic translocase 1 (TL-1) inhibitors developed as potential treatments for mycobacterial diseases or bacterial pneumonia (Streptococcus pneumoniae). TL-1 is a unique antibacterial target, an enzyme required for cell wall synthesis in all bacteria. SQ641 possesses exceptional activity against all members of the Mycobacteria family of bacteria, including M. tuberculosis, M. avium complex, and M. avium subspecies paratuberculosis, the potential etiological agent of Crohn’s disease.
Clostridium difficile Infection
The potential U.S. market for a new drug to eradicate C. difficile is estimated to be $200-$300M. SQ109 has activity in vitro against C. difficile, the infectious  agent responsible for over 50% of all hospital acquired infections and affecting nearly 700,000 patients in the U.S. C. difficile bacteria colonize the GI tract after all normal gut flora are killed off while the patient is on a multi antibiotic regimen. Each year in the U.S., more than 28,000 people die of C. difficile; with 65,000 hospital acquired, hospital onset cases, 50,000 hospital acquired, post-discharge cases, and 263,000 nursing home-onset cases, resulting in $4 billion in excess costs. -
agent responsible for over 50% of all hospital acquired infections and affecting nearly 700,000 patients in the U.S. C. difficile bacteria colonize the GI tract after all normal gut flora are killed off while the patient is on a multi antibiotic regimen. Each year in the U.S., more than 28,000 people die of C. difficile; with 65,000 hospital acquired, hospital onset cases, 50,000 hospital acquired, post-discharge cases, and 263,000 nursing home-onset cases, resulting in $4 billion in excess costs. -

